
Establishing a system to manage payment plans and implement them correctly is important. Checking coverage and gaining pre-approval from insurance companies before treatment helps avoid denials and speeds up payment. Staff TrainingAridness in staff training directly affects how efficiently staff can operate the A/R process. The staff needs regular training to master billing procedures and coding guidelines to handle denial management activities effectively. Claims SubmissionThe health insurance providers receive the electronically submitted coded claims.
Reduced overdue payments
- Provide them with a breakdown of their financial responsibilities, such as copays, outstanding balances, or deductible amounts.
- This step involves collecting and verifying insurance details, contact information, and payment responsibilities.
- If the healthcare providers don’t get payments for months or the payment gets constantly delayed, then it is called aging AR.
- This elasticity ensures consistent service levels while avoiding the overhead of maintaining excess in-house capacity.
- Over 74% of healthcare providers now report an increased financial burden on patients.
After you receive the payment for your rendered service against a claim, the account is no longer in A/R. Our team tracks payments and follow-up on claims, working tirelessly to expedite the insurance reimbursement process, improving your practice’s cash flow. However, if you unnecessarily write off payments, that you can recover through effective A/R management, you will strain your practice’s revenue cycle. The accounts receiver officer (ARO) is responsible for follow-ups and tracking each payment to ensure a steady cash flow. It involves monitoring outstanding balances, initiating follow-up communications, and resolving discrepancies. They play an integral role in revenue cycle management (RCM)Medical Billing by directly affecting the healthcare organization’s sustainability and financial health.
Step 5: Process Improvement

AR in medical billing stands for Accounts Receivable — the money your practice is owed by insurance payers and patients after services are provided. Understanding Accounts Receivable is crucial for smooth operations, timely payroll, and quality patient care. An AR aging report categorizes outstanding payments based on the length of time they have been due, such as 0–30 days, 31–60 days, and beyond. By reducing AR days (the average time taken to collect payments), healthcare providers can improve their revenue cycle and profitability. Insurance AR in medical billing involves claims submitted to payers with contractual agreements, requiring specific follow-up protocols, appeal processes, and payer relationship management. Patient accounts receivable involves individual consumers requiring different communication approaches, payment options, and potentially different collection timelines.
Recover Overdue Payments
In this weblog, I will break down what AR Days mean, how they’re calculated, and why they are crucial for healthcare practices. Let’s present techniques to lessen AR Days and optimize sales cycle management. Use of technology like the RCM software can help your practice automate processes, reduce errors, and improve overall efficiency.
Most medical practices aim for A/R days under 30 to maintain a strong cash flow. However, specialty practices with complex claims may have slightly higher A/R days. AR Aging is a metric used in healthcare RCM to track the age of outstanding accounts receivable. As a report, it categorizes the outstanding invoices by the length of time they have remained unpaid, which is typically in 30-day increments. Paying employees, covering operating expenses, and investing in improved patient care technologies are all made possible by prompt reimbursement.
AR calling helps accounts receivable log for individual patients medical practices ensure that they receive payments for services provided in a timely manner. By following up with patients or insurance companies, medical billing professionals can identify and address any outstanding balances promptly. A medical practice depends on proper accounts receivable management to stay financially secure as well as sustainable. The CMS-1500 form has one main purpose, which is enabling health care providers to bill private insurers and government programs like Medicare and Medicaid. Key information such as patient demographics, medical diagnosis information, and services rendered are included, including procedure codes (CPT/HCPCS) and charges. In medical practices, Accounts Receivable (AR) is a critical function that involves tracking and managing the payments owed by patients and insurance companies for services provided.
- Besides, developing a weekly batch-checking process can also speed up your entire billing workflow.
- The best practice is to verify patient insurance details, including coverage limits, copays, deductibles, and policy expiration dates before they book an appointment.
- With their comprehensive solutions and experienced team, they can help you tackle AR challenges efficiently and optimize your revenue cycle.
- Claims that are lingering in your aging bucket for months are likely to be adjusted or denied, and may be worth very little in terms of reimbursement.
- Patients will likely seek services from a provider who offers more flexibility.
- This may involve investigating any issues with payments, working with clients to rectify any errors, and ensuring that all payments are processed accurately.
- By prioritizing AR follow-up, the medical billing process becomes more efficient.
What are common challenges in AR management?
Join hundreds of practices benefiting from our proven AR management solutions. A delay at any of these junctures can result in “aging AR,” known in lay terms as “overdue balances.” An even worse outcome is petty cash a write-off…revenue that is never captured. Identify common denial trends and correct root causes to prevent recurring issues.

What is Accounts Receivable (A/R) in Healthcare?
Timely collection of payments helps ensure that the practice has the funds necessary to cover operating expenses and provide quality patient care. Opening Entry Medical billing depends strongly on accounts receivable as an essential part. A healthcare provider sees A/R as payment they expect from patients for delivered medical treatment. Medical practices need to handle A/R operations properly to stay financially healthy and operational. This blog article discusses medical billing accounts receivable details including its significance to medical practices and outlines optimal management procedures. In the context of healthcare, AR management involves tracking claims, identifying delayed or denied claims, and following up to ensure timely payment.
Trusted Industry Leader
Outsourcing Accounts Receivable (AR) in medical billing services can greatly benefit both the insurance company and healthcare provider by ensuring a streamlined and efficient claims process. Ideally, a medical claim should be submitted within 72 hours after the service has been provided. If your collections are getting delayed and overdue payments are piling up, it increases days in AR – the average time taken for a claim to be paid based on average daily charge volume.
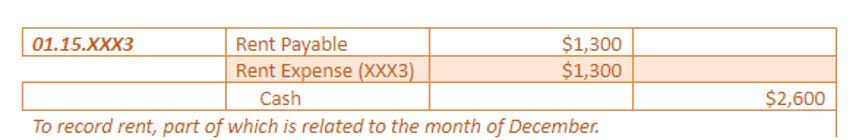
0 responses on "AR Scenarios in Medical Billing: Key Solutions"